Top 2 Thyroid Conditions: Hypothyroidism vs. Hyperthyroidism
September 18, 2024
We ensure our content is always unique, unbiased, supported by evidence. Each piece is based on a review of research available at the time of publication and is fact-checked and medically reviewed by a topic expert.
Written by: Kyla Reda & Heather Schofield
Medically reviewed by: Lara Zakaria PharmD, CNS, IFMCP
Thyroid issues affect around 5% of Americans and 10% of Canadians. (Beynon 2016)(Reyes Domingo 2019)(Statistics Canada 2010) While occurring in both women and men, thyroid conditions are found to be seven times more common in women. (Statistics Canada 2010)(Thyroid Foundation of Canada n.d.) Hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) are the most prevalent thyroid disorders, either producing too little or too much thyroid hormone. (Beynon 2016) Continue reading to learn about the diet and thyroid treatment strategies that may positively impact metabolism and overall well-being.
The thyroid is one of the largest endocrine glands in the body. This small butterfly-shaped organ sits in front of the windpipe (trachea) in the neck and weighs 20–30 g. (Mescher 2010)
The thyroid secretes thyroid hormones, essential for regulating metabolism and body temperature, influencing growth and development, and controlling calcium levels in the blood. (Mescher 2010)
The thyroid gland is responsible for several functions, including:
Controlling the rate at which calories are burned and maintaining muscle function and bone health
Producing heat and energy in the body and increasing metabolic activity
Regulating the development and functioning of the central and peripheral nervous systems, which influences cognitive function, mood, and overall neurological health
Regulating the heartbeat and how much blood goes into circulation
Regulating the speed at which food moves through the digestive tract (Bernal 2022)(Beynon 2016)(Hershman 2020)(Thyroid Foundation of Canada n.d.)
Normal thyroid function is maintained through the hypothalamic-pituitary-thyroid (HPAT) axis, a feedback loop involving the hypothalamus, anterior lobe of the pituitary gland, and adrenal glands.
When thyroid hormone levels are low, the hypothalamus releases thyroid-releasing hormone (TRH) to stimulate the pituitary to release thyroid-stimulating hormone (TSH). The thyroid responds to TSH by producing and secreting more triiodothyronine (T3) and thyroxine (T4) hormones into blood circulation.
When T4 arrives at the targeted body tissue, an iodine derivative (5-iodinase) converts T4 into its more bioactive form, T3. This regulates metabolism and body temperature, generates and absorbs glucose for energy, and increases blood output from the heart. (Beynon 2016)(Costanzo 2010)(Humphreys 2020)(Thyroid Foundation of Canada n.d.)
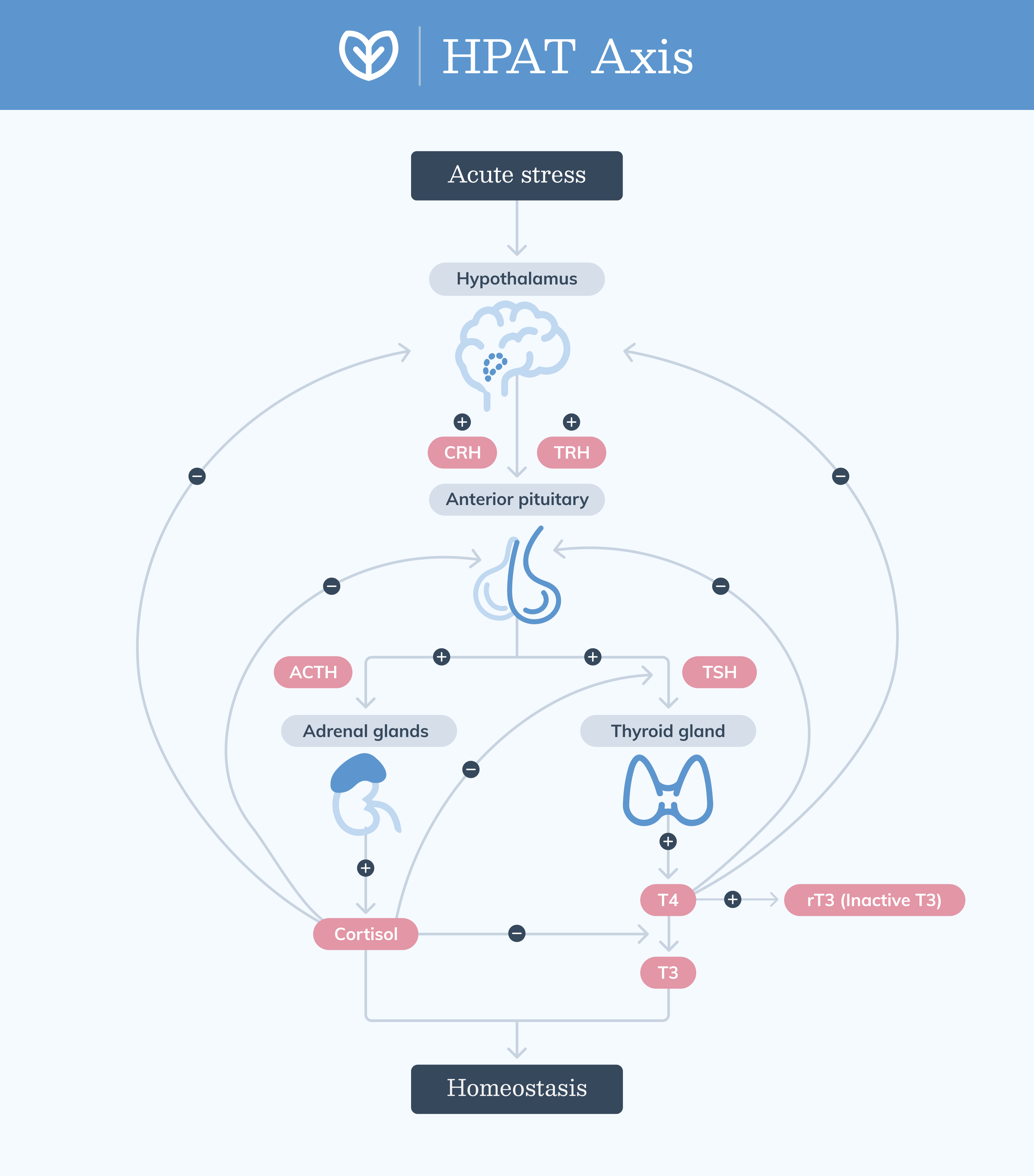 The HPAT axis is a feedback loop used to maintain healthy thyroid hormone levels in the body. (Stephens 2012)
The HPAT axis is a feedback loop used to maintain healthy thyroid hormone levels in the body. (Stephens 2012)
Thyroid disorders affect up to 5% of the population, with hypothyroidism and hyperthyroidism being the most common. (Beynon 2016)(Costanzo 2010)(Golden 2009)
If left untreated, they can increase the risk of adverse cardiac events and high blood pressure, elevated cholesterol, brittle bones, muscle weakness, peripheral neuropathy, cognitive impairment, and infertility. (Duyff 2000)(Gaitonde 2012)(Kravets 2016)(Reyes Domingo 2019)
Thyroid assessment may include looking at the patient’s medical history, performing a physical exam, and thyroid function testing. Treatment goals include returning thyroid levels to normal levels and preventing long-term complications. (BC Guidelines 2018)(Gaitonde 2012)(Kravets 2016)(NIDDK 2016)(NIDDK 2016)
Hyperthyroidism, a condition that affects approximately 1.3% of the population, occurs when the thyroid gland produces and secretes too much thyroid hormone. (Golden 2009)(Hollowell 2002)
Common causes of hyperthyroidism include:
Excessive iodine consumption
Grave’s disease (an autoimmune condition characterized by the destruction of thyroid tissue)
Goiter (enlargement of the thyroid gland causing overproduction of thyroid hormones)
Overmedicating with thyroid hormone replacement therapy
Pituitary abnormalities, such as noncancerous (adenoma) tumors causing too much TSH
Thyroid nodules (cysts or nodules causing overproduction of thyroid hormone)
Thyroiditis (inflammation of the thyroid gland causing too much then too little thyroid hormone) (Beynon 2016)(Duyff 2000)(Golden 2009)(Kravets 2016)(Thyroid Foundation of Canada n.d.)
In the early stages, symptoms of hyperthyroidism may be gradual or develop suddenly. Signs and symptoms include restlessness and difficulty sleeping, weight loss, eye issues, and hot body temperature.
Common symptoms in women and men include:
Difficulty putting on weight, despite increased appetite
Dry and red eyes, the appearance of bulging eyes
Enlarged thyroid gland (goiter)
Excessive sweating
Fast heartbeat (palpitations)
Frequent bowel movements or diarrhea
Heat sensitivity
High (systolic) blood pressure
Mood swings, irritability, and anxiety
Nervous energy
Restlessness and difficulty sleeping
Shaky, tremors, and trembling
Weight loss (BC Guidelines 2018)(Duyff 2000)(Kravets 2016)(NIDDK 2016)(Reyes Domingo 2019)(Vincent 2013)
 Hypothyroidism and hyperthyroidism are the two most common forms of thyroid dysfunction.
Hypothyroidism and hyperthyroidism are the two most common forms of thyroid dysfunction.Hypothyroidism, affecting 4.6% of the population, results when the thyroid gland does not produce and secrete enough thyroid hormone. (Golden 2009)(Hollowell 2002)
Common causes of hypothyroidism include:
Certain medications, including amiodarone, interferon alpha, lithium, and interleukin-2 (NIDDK 2016)
Congenital hypothyroidism (babies born with an underdeveloped or under-functioning thyroid)
Hashimoto’s thyroiditis (chronic inflammation and destruction of the thyroid tissue)
Iodine deficiency
Pituitary abnormalities
Radiation treatment, which can destroy thyroid cells resulting in too little thyroid hormone
Secondary hypothyroidism (the pituitary gland fails to produce enough TSH)
Surgical removal of part or all of the thyroid gland, resulting in too little thyroid hormone
Thyroiditis (Beynon 2016)(Duyff 2000)(Gaitonde 2012)(Golden 2009)(NIDDK 2016)(Thyroid Foundation of Canada n.d.)
In the early stages, symptoms may be mild with a gradual onset. Signs and symptoms of hypothyroidism are similar in both women and men and include fatigue, weight gain, hair loss, and chilliness.
Common symptoms in women and men, include:
Brittle, thinning hair, and hair loss
Constipation
Depression
Dry skin
Enlarged thyroid gland (goiter)
Erectile dysfunction
Eyebrow thinning (outer third)
Hoarseness and feelings of fullness in the throat
Hormonal issues
Infertility
Irregular or heavy periods
Low libido
Memory problems
Muscle aches and weakness
Sensitivity to cold
Slow heart rate
Tiredness or fatigue
Weight gain (BC Guidelines 2018)(Beynon 2016)(Duyff 2000)(Gaitonde 2012)(Reyes Domingo 2019)(NIDDK 2016)(Vincent 2013)
Subclinical (borderline) hypothyroidism affects up to 10% of the adult population. (Biondi 2019) It’s more common in women and usually presents with no symptoms.
Clinically, it’s observed with an elevated TSH and normal free T4 levels. If left untreated, 2–5% of subclinical hypothyroidism cases can progress to symptomatic hypothyroidism. (BC Guidelines 2018)(Khandelwal 2012)(Pearce 2013)
Assessing thyroid function and identifying thyroid disorders require a combination of clinical evaluation and lab testing. Some of the most relevant thyroid tests are listed below.
The TSH test is often the first step in assessing thyroid function. It measures the level of TSH in the blood. High TSH levels indicate hypothyroidism, as the pituitary gland produces more TSH to stimulate an underactive thyroid. Low levels suggest hyperthyroidism, as the pituitary gland reduces TSH production in response to excessive thyroid hormone levels. (NIDDK 2023)
The free T4 test measures the level of unbound T4 in the blood, which is the active form of the hormone. This test helps to confirm the diagnosis suggested by the TSH test. High free T4 levels indicate hyperthyroidism, while low levels suggest hypothyroidism. (NIDDK 2023)
These tests are used to diagnose autoimmune thyroid conditions. Elevated levels of thyroid peroxidase antibody (TPOAb) and thyroglobulin antibody (TgAb) can both indicate Hashimoto’s thyroiditis. High levels of thyroid-stimulating immunoglobulin (TSI) can suggest Graves’ disease. (MedlinePlus n.d.)
Free T3 is the measure of the most biologically active form of thyroid hormone which is free and unbound to carrier proteins. Low free T3 levels can suggest impaired conversion of T4 into T3, often seen in chronic stress or illness. This is often accompanied by elevated reverse T3 (rT3) levels. (DeGroot 2015)(Yamazaki 2021)
The rT3 test measures the level of rT3, an inactive form of T3. It can be useful in certain cases to evaluate thyroid function and metabolism. High levels may indicate non-thyroidal illness syndrome or issues with thyroid hormone conversion. (Frölich 2021)
A thyroid ultrasound is an imaging test that uses sound waves to create pictures of the thyroid gland. It’s useful for detecting nodules, cysts, and structural abnormalities, and to help determine if they may become cancerous. (NIDDK 2023)
When formulating patient treatment plans, diet is an important factor to consider. Thyroid health can be supported by eliminating specific foods and encouraging a quality diet rich in whole foods.
Various whole, unprocessed foods contain thyroid-friendly nutrients, including:
Fruits and vegetables (Kaličanin 2020)
Gluten-free grains and pseudograins (e.g., oats, brown rice, quinoa) (Kravets 2016)(National Institutes of Health 2020)
Healthy fats (e.g., plant oils, extra virgin olive oil) (Kaličanin 2020)(Pang 2021)
Lean meats, fish, and eggs (Kaličanin 2020)(National Institutes of Health 2020)(National Institutes of Health 2020)(National Institutes of Health 2020)
Nuts and seeds (excluding peanuts) (Kaličanin 2020)(National Institutes of Health 2020)(National Institutes of Health 2020)
 Thyroid-friendly foods include lean meats, fish and seafood, eggs, a variety of fruits and vegetables, legumes, nuts and seeds, and healthy fats.
Thyroid-friendly foods include lean meats, fish and seafood, eggs, a variety of fruits and vegetables, legumes, nuts and seeds, and healthy fats.
Specific minerals are needed to maintain thyroid gland function and essential for overall thyroid health. (Ambooken 2013)(Kralik 1996)(Negro 2008)(Ventura 2017)(Wu 2015)(Zimmermann 2015) Zinc, selenium, and iodine can be obtained in the diet by consuming thyroid-friendly foods, including:
Zinc-rich foods: oysters, beef, crab, lobster, baked beans, pumpkin seeds, cashews, almonds, kidney beans, eggs, green peas, dark chocolate (National Institutes of Health 2020)
Selenium-rich foods: brazil nuts, tuna, halibut, sardines, beef, turkey, chicken,brown rice, eggs, baked beans, lentils, cashews, green peas (National Institutes of Health 2020)
Iodine-rich foods: seaweed, dulse, kelp, cod, yogurt, oysters, eggs, liver, cheddar cheese, shrimp, iodine enriched breads and salt (National Institutes of Health 2020)
The thyroid gland is a small but mighty organ, influencing the entire body. Understanding lab test options for thyroid assessment is key to making an accurate diagnosis. Once a clear diagnosis is established, considering dietary intervention strategies is a great way to support patient thyroid health overall.


References
Ambooken, B., Binitha, M, Sarita, S. (2013). Zinc deficiency associated with hypothyroidism: an overlooked cause of severe alopecia. Int J Trichology. 5(1), 40-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746228/
BC Guidelines.ca. (2018). Thyroid function testing in the diagnosis and monitoring of thyroid function disorder. https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/thyroid-testing
Bernal, J. (2022). Thyroid Hormones in Brain Development and Function. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK285549/
Beynon, M.E., Pinneri, K. (2016). An overview of the thyroid gland and thyroid-related deaths for the forensic pathologist.Acad Forensic Pathol. 6(2), 217–236. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6507001/
Biondi, B., Cappola, A.R., Cooper, D.S. (2019). Subclinical hypothyroidism: A review. JAMA. 322(2), 153-160. https://pubmed.ncbi.nlm.nih.gov/31287527/
Carani, C., Isidori, A.M., Granata, A., et al. (2005). Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. The Journal of Clinical Endocrinology & Metabolism. 90(12). https://pubmed.ncbi.nlm.nih.gov/16204360/
Costanzo L.S. (2010). Thyroid Hormones.Physiology. 4th ed. Philadelphia. Saunders Elsevier. p. 401–9. https://search.worldcat.org/title/physiology/oclc/1036817578
DeGroot, L.J. (2015). The Non-Thyroidal Illness Syndrome. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK285570/
Duyff, R.F., Van den Bosch, J., Laman, D.M., et al. (2000). Neuromuscular findings in thyroid dysfunction: A prospective clinical and electrodiagnostic study. Journal of Neurology, Neurosurgery & Psychiatry. 68, 750-755. https://pubmed.ncbi.nlm.nih.gov/10811699/
Frölich, E., & Wahl, R. (2021). Physiological role and use of thyroid hormone metabolites - Potential utility in COVID-19 patients. Frontiers in Endocrinology, 12. https://doi.org/10.3389/fendo.2021.587518
Gaitonde, D.Y., Rowley, K.D., Sweeney, L.B. (2012). Hypothyroidism: An update. Am Fam Physician. 86(3), 244-251. https://www.aafp.org/pubs/afp/issues/2012/0801/p244.html
Golden, S.H., Robinson, K.A., Saldanha, I., et al. (2009). Prevalence and incidence of endocrine and metabolic disorders in the United States: A Comprehensive Review. Journal of Clinical Endocrinology Metabolism. 94(6), 1853-1878. https://pubmed.ncbi.nlm.nih.gov/19494161/
Hershman, J.M. (2020). Overview of the thyroid gland. Merck Manual: Consumer Version. https://www.merckmanuals.com/home/hormonal-and-metabolic-disorders/thyroid-gland-disorders/overview-of-the-thyroid-gland
Hollowell, J.G., Staehling, N.W., Flanders, W.D, et al. (2002). Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 87(2), 489–499. https://pubmed.ncbi.nlm.nih.gov/11836274/
Humphreys, J. (2020). Considerations in evaluating the thyroid gland in a primary care setting.J Family Med Prim Care. 9(12), 5833–5836. https://pubmed.ncbi.nlm.nih.gov/33681003/
Kaličanin, D., Brčić, L., Ljubetić, K., et al. (2020). Differences in food consumption between patients with Hashimoto's thyroiditis and healthy individuals. Scientific reports, 10(1), 10670. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7327046/
Khandelwal, D., & Tandon, N. (2012). Overt and subclinical hypothyroidism: who to treat and how. Drugs, 72(1), 17–33. https://pubmed.ncbi.nlm.nih.gov/22191793/
Kralik, A., Eder, K., Kirchgessner, M. (1996). Influence of zinc and selenium deficiency on parameters to thyroid hormone metabolism. Horm Metab Res. 2(8), 223-226. https://pubmed.ncbi.nlm.nih.gov/8738110/
Kravets, I. Hyperthyroidism: Diagnosis and treatment. (2016). Am Fam Physician. 93(5), 363-370. https://www.aafp.org/pubs/afp/issues/2016/0301/p363.html
Mahmoodianfard, S., Vafa, M., Golgiri, F. et al. (2015). Effects of zinc and selenium supplementation on thyroid function in overweight and obese hypothyroid female patients: A randomized double-blind controlled trial. J Am Coll Nutr. 34(5), 391-9. https://pubmed.ncbi.nlm.nih.gov/25758370/
Maxwell, C., Volpe, S,L. Effect of zinc supplementation on thyroid hormone Function. (2007). Annals of Nutrition and Metabolism. 51, 188-194. https://pubmed.ncbi.nlm.nih.gov/17541266/
MedlinePlus. (n.d.). Thyroid antibodies. National Library of Medicine. https://medlineplus.gov/lab-tests/thyroid-antibodies/
Mescher A.L. (2010). Junqueira's basic histology text & atlas. 12th ed. New York: McGraw-Hill Medical;. Chapter 20, Endocrine glands; 348–70. https://accessmedicine.mhmedical.com/content.aspx?bookid=2430§ionid=190286606
Negro, R. (2008). Selenium and thyroid autoimmunity. Biologics. 2(2), 265–273. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2721352/
NIDDK. (2023). Thyroid tests. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diagnostic-tests/thyroid
Pang, K-L., Lumintang, J.N., Chin, K-Y. (2021). Thyroid-modulating activities of olive and its polyphenols: A systematic review. Nutrients. 13(2), 529. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7915253/
Pearce, S.H.S., Brabant, G., Duntas, L.H., Monzani, F., Peeters, R.P., Razvi, S., et al. (2013) ETA guideline: Management of subclinical hypothyroidism. Eur Thyroid J. 2(4), 215–28. https://pubmed.ncbi.nlm.nih.gov/24783053/
Reyes Domingo, F., Avey, M. T., & Doull, M. (2019). Screening for thyroid dysfunction and treatment of screen-detected thyroid dysfunction in asymptomatic, community-dwelling adults: a systematic review. Systematic reviews, 8(1), 260. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-019-1181-7
Statistics Canada. (2010). Table 13-10-0466-01 Healthy aging indicators. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310046601
Stephens, M. A., & Wand, G. S. (2012). Stress and the HPA axis: Role of glucocorticoids in alcohol dependence. Alcohol Research Current Reviews, 34(4), 468–483. https://pubmed.ncbi.nlm.nih.gov/23584113/
Thyroid Foundation of Canada. (n.d.). www.thyroid.ca
US Department of Health and Human Services: National Institute of Diabetes and Digestive and Kidney Diseases. (2016). Hyperthyroidism. https://www.niddk.nih.gov/health-information/endocrine-diseases/hyperthyroidism
US Department of Health and Human Services: National Institute of Diabetes and Digestive and Kidney Diseases. (2016). Hypothyroidism. https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism
US Department of Health and Human Services: National Institutes of Health, Office of Dietary Supplements. (2020). Iodine, Fact Sheet for Health Professionals. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/
US Department of Health and Human Services: National Institutes of Health, Office of Dietary Supplements. (2020). Selenium, Fact Sheet for Health Professionals. https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
US Department of Health and Human Services: National Institutes of Health, Office of Dietary Supplements. (2020). Zinc, Fact Sheet for Health Professionals. https://ods.od.nih.gov/factsheets/Zinc-HealthProfessional/
Ventura, M., Melo, M., & Carrilho, F. (2017). Selenium and thyroid disease: From pathophysiology to treatment.International journal of endocrinology, 2017, 1297658. https://pubmed.ncbi.nlm.nih.gov/28255299/
Vincent, M., Yogiraj, K. (2013). A descriptive study of alopecia patterns and their relation to thyroid dysfunction. Int J Trichology. 5(1), 57–60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746235/
Wu, Q., Rayman, M.P., Lv, H. (2015). Low population selenium status is associated with increased prevalence of thyroid disease. J Clin Endocrinol Metab. 100(11), 4037-47. https://pubmed.ncbi.nlm.nih.gov/26305620/
Yamazaki, Y., Shoji, T., Miyashima, M., et al. (2021). Low free triiodothyronine level as a Predictor of Cardiovascular Events and All-Cause Mortality in patients undergoing hemodialysis: The DREAM Cohort. Journal of Atherosclerosis and Thrombosis, 28(10), 1071–1082. https://doi.org/10.5551/jat.60624
Zimmermann, M.B., Boelaert, K. (2015). Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 3(4), 286-95. https://pubmed.ncbi.nlm.nih.gov/25591468/